Ahhhhh - Yosemite! What a setting for our 16th (?!?!) annual Manus meeting. We had a strong showing, with 18 participants: Kristin, Tom, Ray, Jon, Randy, Marc, Peter, Sunjay, Lou, Sanj. Bauback, Steve, Warren, Jeff, Jeff, Subir, Milan, and Becky.
Many members arrived on the West Coast early and spent some time in the San Francisco Bay area before heading to Yosemite. Our setting was the beautiful Rush Creek Lodge just outside the valley. The final approach to Rush Creek was a little hairy, but all made it safe and sound!
Steve led us off with a presentation about the use of high resolution ultrasound for the evaluation of radial nerve pathology adjacent to metallic hardware. Ultrasound can determine the continuity of the nerve, whether there is compression from hardware, presence of a neuroma, or just scar tissue. But you’d need a specialized ultrasonographer, someone trained in hydrodissection, probably something that cannot be done in a non-university facility?
In one study: 100% of 13 patients with radial nerve palsy with hardware had an injury at the site of the metal and was identified with ultrasound. The site was marked pre-op by ultrasound before secondary surgery. This is compared to 57% that were accurately identified by MRI.
Can use Checkpoint surgical intra-op to test the nerve. (0.5 is normal. 2 will recover)
Questions: Can you do it yourself? Would it take up to much time in clinic? Do you have enough skill to be certain? With this knowledge, are we obligated to send patients to a facility with a specialized ultrasonographer?
Rob talked about the treatment of bidirectional ligament instability in the elbow. It is difficult to tension both sides properly, simultaneously with a single long tendon graft. Instead, you can use the CLRD (cylindrical ligament retention device) that he first showed us last year when demonstrating his total elbow. The drill has to be perfectly aligned - use the guide to obtain proper valgus alignment and axis of rotation. The ideal tension is 80N. (Average max pull of an ortho resident: 99N!)
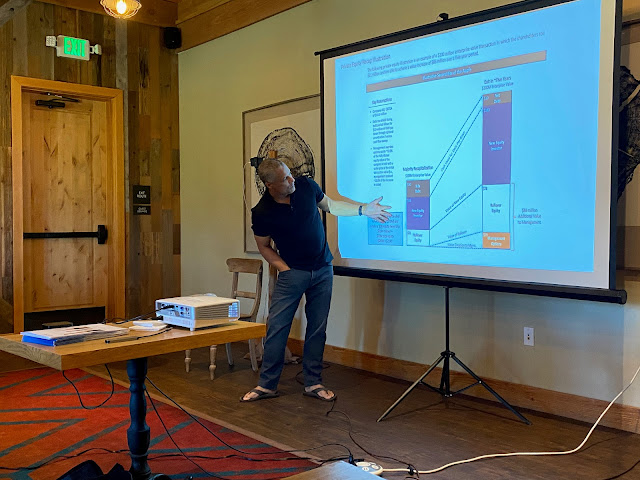
Ray‘s talk about Private Equity was put off due to time constraints. Instead, Milan told us of his experience working with a private equity company for his practice. His advice: have all your ducks in a row when a buyer comes along. Carefully select who you partner with.
Keys: maintain control and maintain independence. For his practice, nothing has changed in the day to day operations. All docs in the practice have to be on board (at least 90-95%) for this to work.
Benefits: monetize your efforts. Get something back for all the work you’ve done over the years. It can give you the opportunity to do something big for the practice, such as adding therapy, increasing EMR capabilities, starting a surgery center, etc.
A new element of the meeting this year was having family come to the meeting room to get breakfast. Over the years we lamented the waste of uneaten food, and some years we had family sneak into the room to grab a muffin. But this year it was made official, and it was nice to see family for a few minutes, confirm plans for the rest of the day, etc. But we had to make it clear that they weren't supposed to sit down and make themselves comfortable! This worked out so well that we have decided to make this a permanent change for future meetings.
Financial independence and the role of real estate.
When your passive income exceeds your living expenses, you have financial independence. Set goals so you define what you are trying to achieve. Things to consider - financial assets, passive income, and what kind of legacy you want to leave. Protect against threats and risks to your plan: taxes, death or disability, third parties, and of course, yourself. To minimize these risks, his recommendation is real estate, specifically, investing through a real estate investment trust (REIT). He recommends the following allocation: 1/3 paper assets (stocks, bonds, etc), 1/3 income producing real estate (at least 10%), 1/3 ownership in a business.
Why real estate? It provides a competitive return to stocks, perhaps with less risk, there is a global market, there is cash flow and growth in the value of the property over time, there is protection against inflation and there are tax advantages.
There are general partners and limited partners, usually split 70/30 or 60/40. Limited partners are not liable for the loan, for managing the property, etc. That falls on the general manager. Limited partners are guaranteed a return of up to 7-8%. Everything above that is split in quarterly distributions. The general partner makes additional compensation, 1-2% management fee, and then a cut of the profits. Sometimes physicians are sought out to be a general partner, borrowing the MD’s net worth.
The key is a property that generates ongoing income through rent and does not depend solely on appreciation. That way you don’t necessarily have to sell the property to make money. These investments are generally recession-resistant, and best in 2nd and 3rd tier communities. IE NOT Manhattan or San Francisco!
Sonex
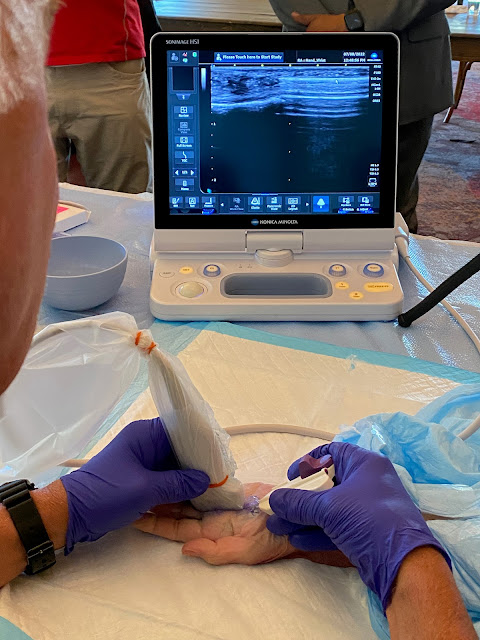
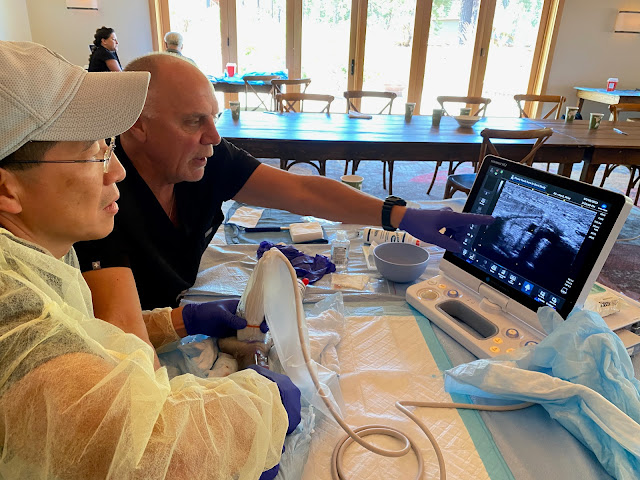
Thank you to our generous sponsors for joining us this week. On Thursday they provided a demonstration of ultrasound-guided carpal tunnel release and trigger finger release. They demonstrated the design of the device and the safety measures built in. For the procedure, start with the bony anatomy, using a rocking, heel-toe motion to identify all structures. Find the transverse safe zone between the hamate or ulnar nerve and the ulnar side of the median nerve. Find the longitudinal safe zone up to the superficial palmar arch. Interestingly, the palmar cutaneous branch is visible 50% of the time, and the motor branch can be seen 100% of the time according to the demo.
Questions and concerns that were raised:
Rob - how safe is the superficial arch? Can you really release distal enough, since incomplete release distally is the most common reason for failure.
Jeff Y - How often is the procedure converted to open? 1 patient that they know of. You can screen with ultrasound ahead of time to be sure all structures can be visualized, and choose the ones who have clearly visualized anatomy.
Jeff F - What is the screen out rate? Depends on experience. No hard data. The idea of “Scanning open house” was floated. How practical is that really?
Ray - What about in patients with previous carpal tunnel release, or established thenar atrophy? They say it can still be done safely, but maybe not for your first few. What do you do as PMR docs? They assured us that they “do not train non-surgeons”.
In the afternoon we retreated to the pool and met up with family. Steve and Ona gave a master class on water polo. Then Steve became a pool toy himself.
We had a happy hour with our Sonex reps followed by the family dinner. I am going to make a plea to everyone, moving forward, to try to get to the happy hour on time, to give our sponsors more time to talk with us before the families descend on the space. While I know he was looking for a way out without being seen, I am grateful to Randy for showing up only a few minutes after I did!
I have absolutely no photos of the beautiful scene of the Manus family gathering for dinner. AND, I just realized that we failed to get a full group photo this year. Oops!
Day 2: July 8
Kristin sent out a survey about practice management. The question was to PA or not to PA? Having a PA or a NP allows increased access to the practice. Most agree they are worth the cost. But you have to invest the time to train them. Essentially you are training them to become you - to talk like you, explain things like you, give examples like you. They do generate revenue in private practice, more in the clinic than in the OR. Most people’s PAs do not go to the OR.
Time to discuss next year’s meeting - in GREECE! Meeting presidents: Subir and Eleni!!
Spouses were invited to sit in on this portion of the meeting - another element that may become a part of our regularly scheduled programming. After yet another discussion about the dates, we decided (again) to keep it the week of July 4. (July 1, 2023 is a Saturday). After reviewing a fabulous and thorough proposal by Ray and Despina, we voted to hold the meeting on Paros, a quiet island but with lots to do and family friendly. There may be a coordinated extended "meeting" to Santorini for a few days afterward. We voted to look for rooms for no more than $750/night. We discussed raising dues - more on that with the Consigliere. Sponsorship - Trimed is still interested. We will ask for $75k from Trimed. If they can’t do the whole thing, we will consider getting a second sponsor to supplement. Maybe Endo again? All expressed excitement at moving forward with this much anticipated meeting. (Damn COVID!)
PAROS
Paros Highlights:
• The Byzantine Museum• Kolymbithres Beach with its moon-like granite rock formations sculpted over millennia by the wind and sea.
• Lively night life
• Beaches for surfing and wind surfing
Let's go!!!!!
Lab: Several ultrasound machines were brought into the room along with cadaver arms for a lab to try the Sonex ultrasound guided CTR and TFR. Many opened the hand after performing the ultrasound guided procedure to confirm that the appropriate anatomic structure had actually been released. The CTR procedure is targeted more toward surgeons who still do only open CTRs, as opposed to those who are doing endoscopic releases, as the benefits are similar between the two.
We were then able to play with some of the ultrasound machines, demonstrating visualization of the ulnar nerve, lateral epicondyle, ganglion cysts, etc.
Friday night we had our adults-only dinner in the private dining room. Delicious salad, short ribs, salmon, brussel sprouts, potatoes. So good I think we actually ran out of food!

Day 3: July 9
Announcements:
Sanj - Hand 22. A series of 22 15-min videos
Topics have already been decided. Let Sanj know if you’re interested in submitting one.
Steve - Handapalooza. Thursday night of ASSH. Member bands playing.
Encourage everyone to go. Gather in a Manus section.
Jeff Y - We are hosting ISSH in DC 2025
Jeffs are involved in the planning. Everyone get involved!
Consigliere Dan Zooming in from home
Dues - Vote to increase dues to $1000 moving forward. Not just for 2023, not just for members going to Greece. Maintain at $500 for 2022. If your dues are not paid, you're out. Pay your dues!
Start documenting more of informal conversations and debates - wait, why are we doing that?
Website - Create bios for each member - 1 paragraph, who, where, who do you teach, who do you influence - add to Manus website. Mostly for sponsors to see who they are connecting with.
Update website with photos, bios, and contact info - working on it!
Bylaws - no more minimum attendance as long as dues are being paid. But we will continue to keep track of attendance because there will be consequences to not attending. Active member not in attendance in person in last 3 years loses veto power. This is big! Our policy had always been that if one member says no to a potential new member, then that person is out. So come to the meetings! Any newly elected member needs to attend the annual meeting within 2 years. Everyone, pay dues by January 31 (fiscal year of the meeting). Virtual attendance does not give attendance credit.
**There will be no virtual option in Greece.**
Membership - have we reached a steady state?
Maintain 30 member cap? No cuts to be made this year. See what happens after dues change to $1000. No dues, out of the club. We did discuss potential new members, but we do not want brand new members to come to Greece. This is a meeting that has been a long time coming, and should be for those who have been committed to the club already.
Potential nominees for 2023 - Ruby Grewal (Jeff F), Tamara Rosental (Warren), Dawn LaPorte, Jim Higgins. Sponsors of potential new members will email the group. Invite them to Handapalooza for meet and greet in Toronto - ASSH annual meeting in 2023. Is everyone good with that? Any issues with these proposed members, or their formal introduction in Toronto in 2023, please email Subir, Kristin, Ray, or Dan if you do not want to discuss with the club as a whole.
Annual meeting - Increase flexibility of the format of the meeting. Change to a 3 or 4 day meeting, without necessarily specifying the days of the week. Increase subsidy for president and treasurer to $2000 for the meeting. (I’m going to throw in a pitch here for something for the secretary too!) We have changed how the president is selected - the new president is no longer the one who nominates the location of the next meeting. Now, we go through the list of those who have not yet served as President. I want to take this opportunity again to congratulate Kristin on a tremendous job this year!
Ray
Benefits of Private Equity
Monetize your practice and achieve sustainability, get something back for your work.Ray described what he is doing to make his practice a part of a total care organization, and something that would be attractive to private equity, but still autonomous. We need strategies to remain independent and relevant. He talked about orthopaedic supergroups, management services organizations, clinical integrated networks, and other things that my little brain cannot quite understand in its entirety without more discussion! I think this is a topic that we should spend more time talking about, as it is something that can likely benefit many of us in the long run.
At the end of the presentation we talked about an idea that came up the night before in the room where it happens. We could develop a Manus fund for commercial real estate purchases. Everything David Blain said sounded great and all, but who has the money to do that?! What about us as a collective buyer? And we could focus on something we know - medical office buildings preferably where members are tenants. Maybe even starting in Berkeley, CA? Let's buy a building for Becky! All who are interested were asked to email Ray with their level of interest both in terms of how much they would want to invest, and whether they want to be a limited or general partner. Collaboration on a whole other level.
Now, back to academics!
Marc led a discussion on radiocarpal fracture-dislocations. He talked about classifications which ideally are used to guide treatment and predict outcome. He described the Moneim and Dumontier classifications.
You need to decide: where is the instability: RC? Intercarpal - VISI vs DISI? DRUJ - Styloid or volar/dorsal ulnar corners? Sometimes it’s all 3. He showed some case presentations and introduced us to the “pooping duck sign” - triquetral avulsion fracture. I am definitely using this one!
• Use spanning bridge plates to support bony and ligamentous repairs
• More bone = more better! Pure soft tissue injury does worse
• Volar-dorsal instability better than radioulnar instability
• Don’t forget associated carpal instability
• Assess for DRUJ instability
Jeff F gave us a primer on injury mechanisms. I enjoyed the presentation so much I am just going to leave you with my outline.
Ballistics
shotgun vs pistol
shotgun multiple pellets, rifle - single missile in shell
hollow point - wrecking ball through tissue
pattern - more spread from rifle the farther away you are, rifle/pistol - single point, longer range
handgun - pistol vs revolver
Accidental discharge while cleaning gun after couple of beers
Blades
knives versus machete
switchblades - illegal in US since 1958. Knife that deploys with a button. Replaced with flipper blade, assisted opening blade
Agricultural implements
auger - large drill bit - move dry material from one place to another, low to high, or drill hole through rock or ice
power take off - connects to tractor transmission (or off your kitchenAid), spins at high speed uncovered - provides power to an attached tool
log splitter - most dangerous when 2 operators get out of sync
winch - cable on a spool. Finger avulsions
lawnmowers and snowblowers
Fireworks
sparklers - individually not dangerous. Sparkler bombs - bunch wrapped together
firecrackers -
roman candles -
rockets
shells and mortars - cause the most destruction. Not meant to be held in hand! Typical split first web space and dislocated thumb CMC. Sometimes tips over and aims the wrong way
homemade
Woodworking tools
saw - blade above (circular saw, miter saw) and blade below (table saw)
Router
Drill press
Lathe
Bauback talked about venous flaps.
Pros: They are thin and pliable, with low morbidity and they are flexible in design. It can be a 1-stage operation. The design can be AVA or AVV. In AVV flaps, you force the blood past the valves, in essence arterializing the veins. This is used for simple coverage rather than revascularization. For revasc, reverse the veins in a AVA design.
The distal forearm is a typical site for harvest. Useful for. many injuries. Examples included fingertip injuries, ATV rollover, flexion contracture from burn, motorcycle accident, wood splitter.
To find veins - Direct visualization, or vein finder (available readily in the OR, NICU, PICU).
Post-operative anticoagulation - just aspirin for outpatient procedures.
Jon
55yo man with left wrist pain. He underwent wrist scope and TFCC repair. On POD 2 a blister on the volar forearm appeared and turned into full thickness forearm burn.
RCA - root cause analysis - was performed. A Linvatec wrist arthroscopy traction tower was used, coban wrap. The tower was warm but the temperature was not excessive. The area of burn was outside the dressing and not where the tower contacted the forearm.
Jon reviewed for us Fourier’s law of thermodynamics. He learned the cooling profile of the tower. Closer followup with patient than normal: dressing changes, debridement, etc. Key: maintain relationship with patient, document everything.
The question here is equipment malfunction versus negligence.
Settlement check on behalf of hospital versus on behalf of you.
Kristin
42 yo woman OB/GYN NP. She presented with a Right trigger thumb and had had 2 prior injections elsewhere. On exam, she had a Right trigger thumb and surgery was scheduled. It was performed in office under WALANT - uncomplicated. Lido with epi was used for local. The finger blanched but then pinked up which is typical. Kristin applied the dressing herself.
On POD 2 the were color changes in the finger, and the patient was sent to the ER. The ER warmed the thumb, color returned, and she was discharged. On POD 3 Kristin called the patient - the thumb had normal color and temp, there was no pain, with improving sensation. She was asked to come in but patient said said she was fine and had no concerns.
On POD 7 color change again, darker. The patient was urgently brought to office. PA assessed. The thumb had been pink earlier that day (KH home with COVID). She was sent to Duke - angiogram, tpa, heparin, hyperbaric oxygen, botox, stellate ganglion block, labs to assess for coagulopathy all considered. Angiogram showed acute cut off at MC.
Munchausen??? How can we know?
During the Tsunami presentations a question came up regarding our role as "consultants" for our colleagues should any of these cases (any cases, not just these 2) go to litigation. Could we be subpoenaed? The determination after a short debate was that we are a “Quality Improvement” team and our discussions here are not discoverable. Does anyone dispute this conclusion?
The 2022 Tsunami winner is: Jon! We are all grateful for Jon and Kristin for sharing their cases with us. Presentation of these Tsunami cases is often the most educational part of this meeting, at least for me. It really helps me to reflect on these discussions whenever I find myself in difficult situations. So thank you, and thanks to everyone who has ever presented their complications. You are greatly appreciated!
We were fortunate in our timing. We had spectacular weather, and gorgeous views from all the hikes throughout the valley. But as we began our meeting, a fire broke out in the Mariposa Grove of Giant Sequoias, endangering the ancient trees, and burning almost 5000 acres of the park. Smoke drifted in and out of the valley, creating a haze over the iconic El Capitan.















.jpeg)
.jpeg)

.png)